Reducing the duration of mechanical ventilation with a statistical theory
A team of researchers from IMT Atlantique has developed an algorithm that can automatically detect anomalies in mechanical ventilation by using a new statistical theory. The goal is to improve synchronization between the patient and ventilator, thus reducing the duration of mechanical ventilation and consequently shortening hospital stays. This issue is especially crucial for hospitals under pressure due to numerous patients on respirators as a result of the Covid-19 pandemic.
Dominique Pastor never imagined that the new theoretical approach in statistics he was working on would be used to help doctors provide better care for patients on mechanical ventilation (MV). The researcher in statistics specializes in signal processing, specifically anomaly detection. His work usually focuses on processing radar signals or speech signals. It wasn’t until he met Erwan L’Her, head of emergencies at La Cavale Blanche Hospital in Brest, that he began focusing the application of his theory, called Random Distortion Testing, on mechanical ventilation. The doctor shared a little known problem with the researcher, which would become a source of inspiration: a mismatch that often exists between patients’ efforts while undergoing MV and the respirator’s output.
Signal anomalies with serious consequences
Respirators–or ventilators–feature a device enabling them to supply pressurized air when they recognize demand from the patient. In other words, the patient is the one to initiate a cycle. Many adjustable parameters are used to best respond to an individual’s specific needs, which change as the illness progresses. These include inspiratory flow rate and number of cycles per minute. Standard settings are used at the start of MV and then modified based on flow rate/ pressure curves–the famous signal processed by the Curvex algorithm, which resulted from collaboration between Dominique Pastor and Erwan L’Her.
Patient-ventilator asynchronies are defined as time lags between the patient’s inspiration and the ventilator’s flow rate. For example, the device cannot detect a patient’s demand for air because the trigger threshold level is set too high. This leads to ineffective inspiratory effort. It can also lead to double triggering when the ventilator generates two cycles for one patient inspiratory effort. The patient may also not have time to completely empty their lungs before the respirator begins a new cycle, leading to dynamic hyperinflation of the lungs, also known as intrinsic PEEP (positive end-expiratory pressure).
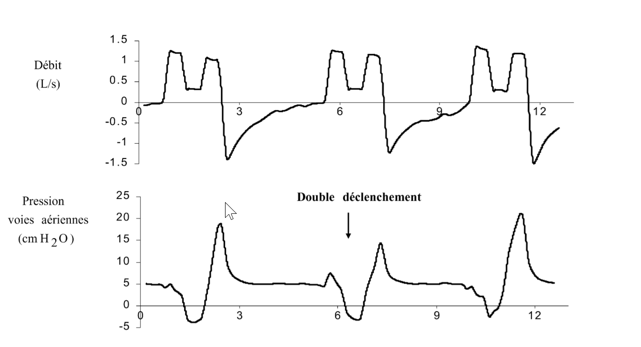
Example of double triggering: a single inspiratory effort results in two ventilator insufflations within a short time span.
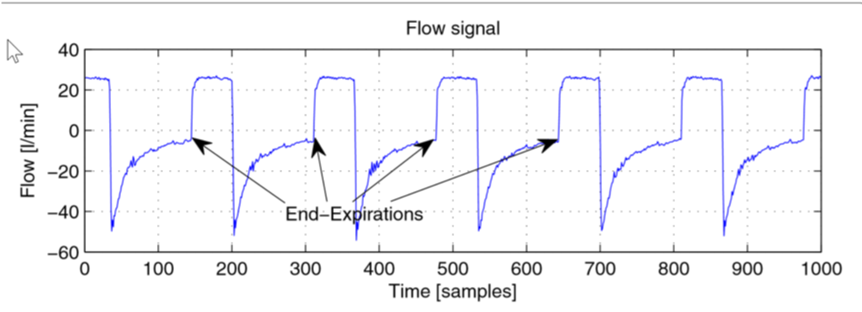
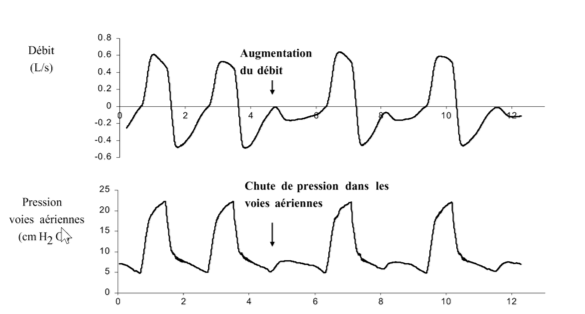
Example of positive end expiratory pressure: the next ventilator insufflation occurs before the flow has returned to zero at the end of expiration.
These patient-ventilator anomalies are believed to be very common in clinical practice. They have serious consequences, ranging from patient discomfort to increased respiratory efforts that can lead to invasive ventilation–intubation. They involve an increase in the duration of mechanical ventilation, with an increase in weaning failure (end of MV) and therefore longer hospital stays.
However, the number of patients in need of mechanical ventilation has skyrocketed with the Covid-19 pandemic, while the number of health care workers, respirators and beds has only moderately increased, which at times gives rise to difficult ethical choices. A reduction in the duration of ventilation would therefore be a significant advantage, both for the current situation and in general, since respiratory diseases are becoming increasingly common, especially with the aging of the population.
A statistical model that adapts to various signals
Patient-ventilator asynchronies result in visible anomalies in air flow rate and pressure curves. These curves model the series of inspiratory phases, when pressure increases and expiratory phases, when it decreases, with inversion of the air flow. Control monitors for most next-generation devices display these flow rate and pressure curves. The anomalies are visible to the naked eye, but this requires regular monitoring of the curves, and a doctor to be present who can adjust the ventilator settings. Dominique Pastor and Erwan L’Her had a common objective: develop an algorithm that would detect certain anomalies automatically. Their work was patented under the name Curvex in 2013.
The detection of an anomaly represents a major deviation from the usual form for a signal. “We chose an approach called supervised learning by mathematical modeling,” Dominique Pastor explains. One characteristic of his Random Distorsion Testing theory is that it makes it possible to detect signal anomalies with very little prior knowledge. “Often, the signal to be processed is not well known, as in the case of MV, since each patient has unique characteristics, and it is difficult to obtain a large quantity of medical data. The usual statistical theories have difficulty taking into account a high degree of uncertainty in the signal. Our model, on the other hand, is generic and flexible enough to handle a wide range of situations.”
Dominique Pastor first worked with intrinsic PEEP detection algorithms with PhD student Quang-Thang Nguyen, who helped to find solutions. “The algorithm is a flow rate signal segmentation method used to identify the various breathing phases and calculate models for detecting anomalies. We introduced an adjustable setting (tolerance) to define the deviation from the model used to determine whether it is an anomaly,” Dominique Pastor explains. According to the researcher from IMT Atlantique, this tolerance is a valuable asset. It can be adjusted by the user, based on their needs, to alter the sensitivity and specificity.
The Curvex platform not only processes flow data from ventilators, but also a wide range of physiological signals (electrocardiogram, electroencephalogram). A ventilation simulator was included, with settings that can be adjusted in real-time, in order to test the algorithms and perform demonstrations. By modifying certain pulmonary parameters (compliance, airway resistance, etc.) and background noise levels, different signal anomalies (intrinsic PEEP, ineffective inspiratory effort, etc.) appear randomly. The algorithm detects and characterizes them. “In terms of methodology, it is important to have statistical signals that we can control in order to make sure it is working and then move on to real signals,” Dominique Pastor explains.
The next step is to create a proof of concept (POC) by developing electronics to detect anomalies in ventilatory signals, to be installed in emergency and intensive care units and used by health care providers. The goal is to provide versatile equipment that could adapt to any ventilator. “The theory has been expanding since 2013, but unfortunately the project has made little progress from a technical perspective due to lack of funding. We now hope that it will finally materialize, in partnership with a laboratory, or designers of ventilators, for example. I think this a valuable use of our algorithms, both from a scientific and medical perspective,” says Dominique Pastor.
By Sarah Balfagon for I’MTech.
Learn more:
– Mechanical ventilation system monitoring: automatic detection of dynamic hyperinflation and asynchrony. Quang-Thang Nguyen, Dominique Pastor, François Lellouche and Erwan L’Her
Illustration sources:



Leave a Reply
Want to join the discussion?Feel free to contribute!